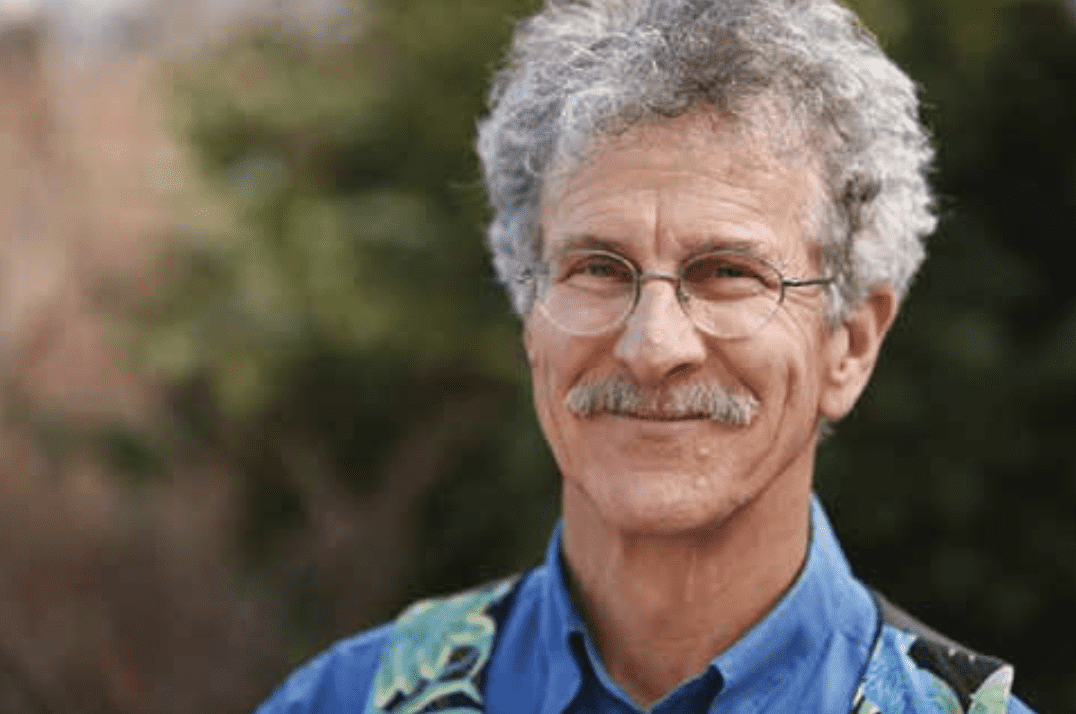
Dr. Marc Heller Keep Moving, Age Gracefully
For 45 years, Dr. Marc Heller has been a trusted figure in Ashland’s healthcare community. A chiropractic physician with deep expertise in lower back issues, Dr. Heller has helped thousands of patients reclaim mobility and reduce chronic pain—especially those who had nearly given up hope. Now, as he shifts his focus to working primarily with older adults, his practice has evolved into something even more refined: gentle, informed, empowering care that emphasizes lasting change. In this interview, Dr. Heller shares insights from his long and varied career, his philosophy on aging and movement, and how the right kind of care can make all the difference.
Hi Dr. Heller, great to have you back and to do this interview with you here today.
Great to be here and to have the opportunity to talk to the community.
Dr. Heller, you’ve been in practice in Ashland for 45 years. How has your work evolved over the decades?
I’ve had at least ten careers within this one. Over the years, I’ve studied everything from traditional chiropractic to energetic medicine, soft-tissue techniques, exercise rehabilitation, and low-force methods—learned primarily from osteopathy. I started out using hands-on, high-force adjustments; now my work is gentler, more precise, and tailored to the needs of older adults. I’ve become a better listener—both to my patients and to their bodies.
You’re known for your expertise in low back pain. What led you to focus so deeply in this area?
It’s personal—I’ve had lower back pain from torn lumbar discs for over 30 years. That pain has been my teacher. It’s helped me become an expert—not just in treatment, but in empathy. The spine is complex. My goal isn’t to “crack” it, but to understand it, gently treat it, and teach my patients how to avoid re-injury.
Chronic lower back pain can have many causes—lumbar discs, sacroiliac joints, the tailbone, lumbar facets, hips, knees, feet, and even the little-known cluneal nerves. When patients have long-term low back pain, their core becomes weak, which only makes the problem worse. Part of my job is to untangle the source of each patient’s pain. You can’t treat it effectively unless you understand where it’s coming from.
What is non-invasive regenerative medicine? Do you offer this?
When you injure yourself, most healing happens within the first six weeks. After that, soft tissues usually stop healing on their own—so finding ways to reawaken the body’s natural repair process is key.
That’s the idea behind non-invasive regenerative medicine, which harnesses the body’s innate healing wisdom to address the root cause of dysfunction and repair damaged tissues. In conventional medicine, this includes treatments like platelet-rich plasma (PRP), prolotherapy, and stem cell therapy.
In my practice, I am lucky to have a Piezo Wave machine—a non-invasive therapy that stimulates soft tissue healing without the need for needles or injections. It’s an amazing tool that’s quite similar in concept to prolotherapy or PRP. There’s great research supporting its use for conditions like plantar fasciitis and shoulder tendonitis, but it’s useful for almost any chronic soft tissue problem. This is not a standalone therapy; it works best when combined with spinal adjustments, other soft tissue therapies, and exercise.
What are the challenges of working with older clients? How is their care unique?
Older bodies are generally stiffer and less flexible, which means they respond best to a gentler, slower form of chiropractic care. It also means that I need to be thoughtful about which flexibility and strength exercises are both safe and effective. Being an older person myself, I understand these challenges firsthand and tailor my approach with that empathy in mind.
Older patients are often told they have degeneration of the spine—a form of arthritis—based on X-rays or MRIs. That’s a very discouraging message. It misses the fact that spinal degeneration, like gray hair and wrinkles, is a normal part of aging. It’s rarely the actual cause of the pain.
Unfortunately, many people with lower back pain never receive a truly accurate diagnosis. I suspect that’s because listening to the patient and performing a hands-on physical exam have become lost arts. In my practice, I focus on assessing function—not just reading X-rays and MRIs—so I can identify what’s really driving the pain.
What happens when older adults receive the wrong diagnosis or treatment?
When older adults receive the wrong diagnosis or treatment, the first and most obvious result is that they rarely get better. Pain becomes chronic, and that ongoing discomfort often leads people to move less. Unfortunately, when you stop moving, you age faster—physically, mentally, and emotionally.
Fear of pain or re-injury can create a cycle of stiffness, pain, and isolation. My role is to help patients break that cycle and reverse the spiral. I want to help people keep active and engaged—safely—for as long as possible. Movement is medicine, and it’s never too late to reclaim it.
You’ve studied with a number of well-known practitioners. Who stands out as a major influence?
I’ve been fortunate to study with many brilliant practitioners, but a few have had a lasting impact. One of my biggest influences is Dr. Stuart McGill, a PhD researcher who has devoted his life to understanding the biomechanics of the spine. His approach—diagnose accurately, treat with precision, and teach self-care—forms the foundation of my work with patients dealing with lower back. I recommend his book, The Back Mechanic, to many patients.
I also learned so much from Dr. Jean Pierre Barral, a French osteopath known for his work in visceral manipulation. He taught me how to listen carefully to what the body has to say—to tune into its subtle rhythms and messages.
A second valuable lesson he imparted was not to ignore the front of the body— particularly the abdomen. Most chiropractors focus on the back of the body, but many muscles that affect posture, breathing, and core stability are located in the front. Barral’s work also addressed movement problems of the abdominal organs themselves.
Another major influence on my approach is the circle of professionals who combine chiropractic adjustments with physical therapy rehab. I’ve studied with so many I can’t name them all, but I’ll shortlist Craig Liebenson, DC; Phillip Snell, DC of Portland Oregon; and Michael Shacklock, PT, an Australian physical therapist who focuses on nerves and how to treat them. Their insights have helped me refine how I approach complex cases and chronic pain.
How do you approach diagnosing back pain differently than many other doctors?
I approach back pain like a detective solving a mystery. My job is to gather clues—by listening to your story, watching how your body moves, and using my hands to uncover what might not show up on a scan.
Too often, the diagnosis of back pain is rushed or overly reliant on imaging. MRIs can be helpful, but they frequently show things like arthritis or disc bulges that aren’t actually causing the pain. In fact, those findings are common even in people who feel just fine. That’s why a hands-on, real-time assessment is so critical. Pain is personal—it needs to be understood in the context of your body, not just a black-and-white image.
I like to rely on what I call the “ancient arts” of diagnosis—taking a good old-fashioned history and performing a physical exam. I ask: Can I touch your pain? Can I reproduce or relieve it through movement or gentle pressure? Does it hurt more when you sit, stand, walk, or bend? By assessing your pain in real time, in your body, I get clues that help me understand what’s really going on—and how to treat it effectively.
What does “self-care” mean when it comes to managing back pain?
Self-care is one of the most important—and often overlooked—parts of managing back pain. I can’t just fix you. Your daily activities are such an important part of you getting well. What you do every day, how you move, sit, stand, and even rest, all play a huge role in whether your body heals or stays stuck in a pain cycle.
Self-care goes beyond just exercise. It’s about learning what to do—and what not to do. For example, yoga can be helpful for some people, but for others who are already hyper-mobile, it may actually make things worse. Movement, posture, nutrition, and body awareness all factor in.
My job is to help people understand their own patterns—what’s helping and what’s hurting—and then give them the tools to break the habits that are causing harm. When patients become active participants in their own healing, that’s when I see real, lasting progress.
How is your approach different?
My approach is all about making you independent—giving you the tools you need to take care of yourself long-term. While I do provide maintenance care, especially for older patients dealing with chronic pain, I prefer a beginning-middle-end approach. Let’s figure out what’s wrong, work together to improve it, and then give you the knowledge and strategies to keep yourself well.
One of my core goals is to move your pain from the center of your life to the sidelines. Not all pain can be completely eliminated—and I’ll always be honest about that—but when you understand what helps and what hurts, you gain a sense of control again. With the right combination of chiropractic, soft tissue work, lifestyle changes, and targeted exercises, you’ll feel so much better.
Are there misconceptions patients often bring into your office?
Yes. One of the biggest misconceptions I see is the belief that someone is broken beyond repair. Many patients come in feeling hopeless because they’ve internalized a diagnosis. They’ll say, “I have arthritis, so I’ll never get better,” or “I guess this pain is just part of getting older. But that’s not necessarily true.
Pain is not an inevitable part of aging, and arthritis is not always painful. In fact, research has shown that the amount of degeneration on an X-ray or MRI doesn’t always match up with how much pain someone feels. Over 50% of people over 60 have spinal degeneration—but only a fraction experience pain. We need to stop equating scary images with permanent decline.
You’re still practicing. What keeps you inspired?
I’m 75 years old, but I’m still practicing because I truly love what I do. I love helping people feel better—especially when they’ve been to multiple providers and still haven’t found relief. There’s something deeply satisfying about helping someone finally turn a corner when no one else could.
I also enjoy the human connection of my work. The relationships I build with my patients—many of which last decades—are deeply meaningful to me.
And the work itself keeps me mentally sharp. I’ve always loved the puzzle of it—figuring out what’s really going on beneath the surface. Diagnosis is like detective work, and when you finally put the pieces together and see someone start to heal, it’s incredibly rewarding. That’s what keeps me inspired after all these years.
Can you share a case or two that exemplifies your current work?
Two recent cases illustrate the kind of work I do. The first was a 47-year-old woman who had been a world-class paraglider. She had suffered a traumatic fall that broke her sacrum and tailbone and caused a herniated L5 disc. She lived with severe pain and disability for five years. After reading some of my articles online, she sought me out. Within a month of treatment, her pain dropped from a constant 8 or 9 out of 10 to a manageable 3. For her, that was life-changing progress.
The second case was a 70-year-old woman who had just moved to the area. She was in constant low back pain and couldn’t find any comfort. But she was committed. She did the work—chiropractic, exercises, lifestyle changes—and within two months, she was pain-free for the first time in years. We were able to release her from care, and she walked away with a renewed sense of ease in her body.
How would you describe your treatment style today?
My treatment style today is slower, gentler, and much more collaborative than it was when I first started out. I don’t “pop” backs or use high-force techniques. I don’t lay people on their sides and thrust into the spine. Instead, I work with the body—listening carefully to what it needs and responding with precision and respect.
Treatment might involve adjusting the spine, or working with the abdomen, the fascia, or other soft tissues that are contributing to pain or dysfunction. I draw from a variety of techniques, depending on what your body is telling me. Every case is unique, so my approach is never one-size-fits-all. It’s about meeting each patient where they are and helping them move forward safely and effectively.
What’s your message to older adults who may be feeling discouraged about their health or mobility?
Don’t give up. Be patient. I know it can be discouraging, especially if you’ve been living with pain or limitations for a long time—but your body is still capable of change. Healing may not be instant, and it may not look the same as it did when you were younger, but meaningful progress is possible at any age.
You just need the right guidance and mindset. Keep moving, keep believing in yourself, and remember—pain doesn’t have to be the center of your life.
Learn More: